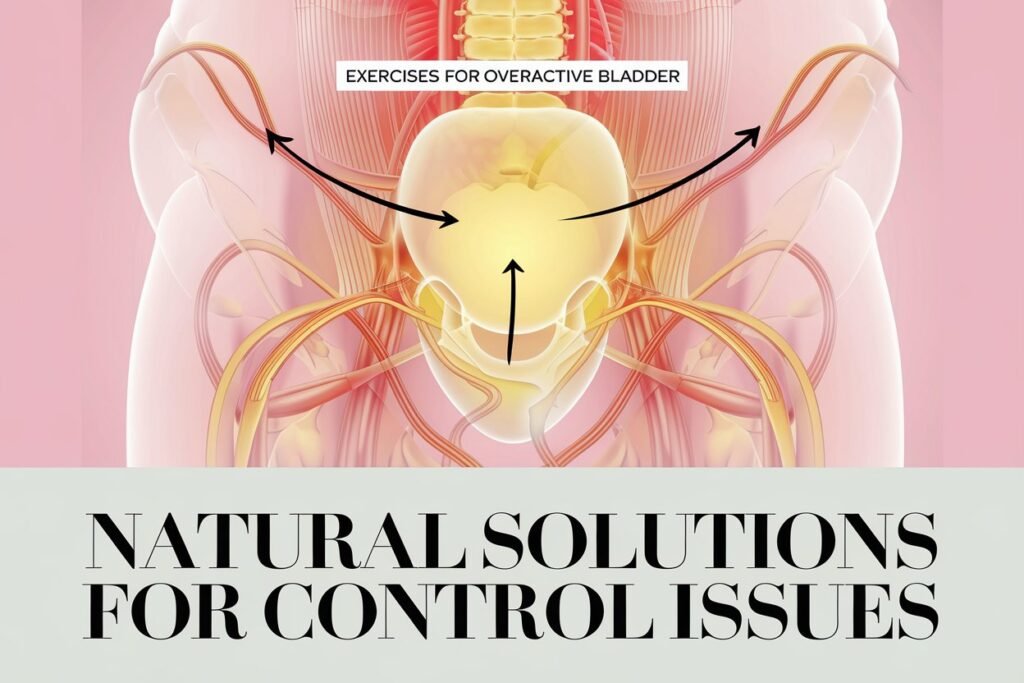
Understanding Overactive Bladder
Overactive Bladder (OAB) is a condition characterized by a range of urinary symptoms that can significantly disrupt an individual’s daily life. The hallmark symptoms include a frequent and urgent need to urinate, often accompanied by incontinence, which can lead to leakage of urine. Individuals with OAB may also experience nocturia, the need to wake up multiple times during the night to urinate. These symptoms can vary in intensity and may arise unexpectedly, causing substantial psychological distress and social embarrassment.
The causes of overactive bladder are multifaceted, with a variety of factors contributing to its development. These can range from neurological disorders, such as multiple sclerosis or stroke, to urinary tract infections, medication side effects, and age-related changes in the bladder’s function. Pelvic floor muscle weakness, particularly in women, can also play a significant role in the onset of OAB, making it essential to consider both physiological and psychological dimensions when addressing the condition.
OAB is a prevalent issue affecting millions worldwide across all demographic groups, though it is more common in older adults and women. Studies suggest that nearly 30% of people aged 65 and older may experience symptoms of OAB, and the prevalence tends to increase with age. Beyond its physical implications, OAB can drastically affect one’s quality of life, leading to social isolation, limitations in daily activities, and heightened anxiety about events wherein restroom access may be limited.
Given these challenges, addressing overactive bladder through comprehensive approaches is vital. Exercises specifically designed to strengthen the pelvic floor muscles can be an effective method, providing individuals with a natural and empowering way to manage their symptoms. Recognizing the importance of this condition and its impact on daily life can pave the way for tailored interventions that enhance overall well-being.
The Role of Exercise in Managing OAB
The management of overactive bladder (OAB) often requires a multifaceted approach, and exercise plays a crucial role in this context. Regular physical activity has been shown to enhance bladder health, primarily through strengthening the pelvic floor muscles. These muscles support the bladder and are pivotal in controlling urination. A strong pelvic floor can significantly reduce the frequency and urgency associated with OAB symptoms.
Research within the field of urology has indicated that individuals engaging in regular exercise experience improved bladder control. A study published in the *Journal of Urology* found that participants who incorporated pelvic floor exercises into their routine reported a noticeable reduction in urgency episodes and an overall increase in quality of life. This evidence underscores the significance of adopting an exercise regimen that targets pelvic muscles, as it not only empowers patients to manage their condition but also enhances their physical well-being.
Additional studies affirm that moderate aerobic exercise, such as walking, swimming, or cycling, can positively impact bladder function. These activities help promote healthy body weight and improve cardiovascular health, which have both been linked to alleviating OAB symptoms. Furthermore, exercises that focus on core strength and stability often improve overall coordination and body awareness, further benefiting bladder control.
Experts recommend that individuals with OAB consider integrating both pelvic floor exercises, commonly known as Kegel exercises, alongside general fitness activities into their routines. While traditional medical treatments for OAB are widely available, adopting a proactive approach through regular exercise can serve as a valuable non-invasive complement. With consistent commitment to an exercise program, many individuals may find significant improvements in their bladder function and fatigue from urgency thus lessened.
Types of Exercises Beneficial for OAB
Individuals dealing with overactive bladder (OAB) often find relief through specific exercises designed to strengthen the pelvic floor and enhance bladder control. Among the most effective methods are Kegel exercises, bladder training, pelvic floor strength training, and low-impact aerobic activities. Each exercise offers unique benefits and is suitable for various individuals.
Kegel exercises are a cornerstone in OAB management. These exercises focus on strengthening the pelvic floor muscles, which support the bladder and urethra. To perform Kegels, one should identify the correct muscles by trying to stop urination mid-flow. Once identified, the individual can contract these muscles for a count of three, then relax for a count of three, gradually increasing the duration as strength improves. Consistent practice can lead to improved bladder control and a reduction in urgency and frequency of leaks.
Bladder training is another valuable technique, designed to increase the interval between urination. This method involves setting scheduled times for bathroom breaks, gradually extending the time between trips to the restroom. This approach can help retrain the bladder, allowing it to hold more urine and reducing the urge to go frequently. It is particularly beneficial for those who experience sudden urges and can be customized based on individual needs.
Pelvic floor strength training includes various exercises that not only enhance the pelvic muscles but also encourage overall core stability. Activities such as bridges or squats performed correctly can help enhance these vital muscles. Low-impact aerobic activities, such as walking or swimming, contribute to overall fitness while minimizing strain on the bladder. These types of activities can further aid in reducing bladder pressure. Engaging in a combination of these exercises can provide comprehensive benefits for individuals seeking to manage OAB symptoms effectively.
How to Perform Kegel Exercises Correctly
Kegel exercises are an effective natural solution for improving bladder control by strengthening the pelvic floor muscles. The first step in performing Kegel exercises correctly is to locate the pelvic floor muscles. These are the muscles you use to stop urination mid-flow. A helpful method to identify them is to try interrupting your urine stream during urination. Once you identify these muscles, it is crucial to ensure they are the ones being engaged outside of the bathroom.
To perform Kegel exercises, follow these steps: Begin by finding a comfortable position, whether sitting or lying down. Relax your body, including your abdominal and thigh muscles, as tension can hinder the effectiveness of the exercise. Once you’re relaxed, contract the pelvic floor muscles as if you are attempting to hold back urine. Maintain this contraction for about three to five seconds, then release and relax for the same duration. Aim for 10 repetitions per session, and gradually increase the count as you become more comfortable with the technique.
When engaging in Kegel exercises, it is essential to focus on the rhythm of contracting and relaxing rather than holding your breath. Keeping a steady breath pattern will aid in the overall relaxation of the muscles. Beginners may find it helpful to start with short holds before progressing to longer contractions, ultimately striving for 10 seconds per hold as strength improves. Common mistakes include using other muscle groups, such as the buttocks or thighs, so it is important to concentrate solely on the pelvic floor.
Incorporating Kegels into your daily routine can lead to significant improvements in bladder control. By practicing consistently, you can develop stronger pelvic floor muscles and reduce symptoms associated with overactive bladder. Always remember that quality matters more than quantity, so aim to perfect the technique before increasing the number of repetitions.
Incorporating Bladder Training into Your Routine
Bladder training is an effective approach for individuals looking to manage overactive bladder symptoms. It encourages the gradual increase of time between bathroom visits, fostering better control of urination. The process begins with establishing a baseline schedule based on your current habits. For example, if you find yourself visiting the restroom every hour, aim to extend this interval gradually. Start by waiting an additional 15 minutes before each subsequent visit. Over time, you can increase this duration as you become more comfortable.
Recognizing your urge patterns plays a key role in bladder training. Individuals are encouraged to pay attention to their body’s signals and note when urges occur. By understanding personal triggers, such as stress or consuming certain beverages, one can develop a tailored schedule that minimizes sudden urges to urinate. Keeping a bladder diary can enhance this process. Documenting the times of bathroom visits, fluid intake, and urgency levels helps in identifying patterns and progress. This record not only serves as a valuable tool for effective communication with healthcare providers but also tracks improvements in bladder control.
Mental techniques can also significantly support bladder training efforts. Positive reinforcement, such as rewarding oneself for successfully extending the intervals between trips to the restroom, can boost motivation. Additionally, practicing mindfulness techniques may help individuals manage anxiety related to urges. Techniques like deep breathing or visualization can enhance relaxation during moments of urgency, reducing the perception of discomfort.
Incorporating these strategies into your daily routine requires patience and commitment. With consistent practice, it is possible to achieve better bladder control and diminish the impact of overactive bladder symptoms on your life. As the adjustments become part of your lifestyle, you may experience increased confidence and an improved quality of life. Ultimately, successful bladder training can provide a foundation for long-term management of overactive bladder issues.
Physical Activities that Support Bladder Health
Maintaining bladder health is crucial for overall well-being, and engaging in physical activities can significantly contribute to managing an overactive bladder. Among the various options available, low-impact exercises like yoga, pilates, swimming, and walking are particularly beneficial for promoting bladder health and enhancing pelvic muscle function.
Yoga is well-known for its calming effects on the mind and body, making it an excellent choice for individuals seeking to alleviate the symptoms associated with an overactive bladder. Through postures and breathing techniques, yoga can help to strengthen the pelvic floor muscles, improving their control and function. Additionally, the relaxation techniques inherent in yoga can aid in reducing anxiety, which, in some cases, may worsen bladder symptoms.
Pilates is another effective physical activity that emphasizes core strength, stability, and alignment. Many pilates exercises specifically target the abdominal and pelvic floor muscles, helping to improve bladder control. By focusing on controlled movements and breathwork, practitioners can enhance their awareness of these crucial muscles, leading to more efficient bladder function.
Swimming offers a low-impact, full-body workout that can also support bladder health. The buoyancy of water reduces stress on the joints, allowing individuals to engage in a range of movements that may be difficult on land. Swimming can promote relaxation and has been shown to help regulate nerve responses, which may positively impact bladder function.
Walking, a simple yet effective physical activity, plays a vital role in maintaining overall health. It is an accessible form of exercise that can be easily incorporated into daily routines. Regular walking can enhance circulation, strengthen muscles, and contribute to weight management, all of which are essential factors for supporting optimal bladder health.
Incorporating these physical activities into a regular routine can yield significant benefits for individuals dealing with bladder concerns. Not only do they promote physical wellness, but they also foster a sense of relaxation and body awareness that can empower individuals to better manage their symptoms.
Lifestyle Changes to Complement Exercises
Overactive bladder (OAB) can significantly impact daily life, making it essential to adopt a comprehensive approach that includes not only targeted exercises but also specific lifestyle modifications. These adjustments can work in harmony with exercise regimens to enhance bladder control and overall well-being.
One of the primary lifestyle changes involves dietary adjustments. Reducing the intake of irritants such as caffeine and alcohol has been shown to mitigate OAB symptoms. Both substances can stimulate the bladder and may increase urgency and frequency of urination. Instead, opting for non-caffeinated beverages and encouraging hydration through water can lead to better bladder health. Furthermore, a well-balanced diet rich in fruits, vegetables, and fibers can assist in maintaining normal bowel function, which is crucial for avoiding added pressure on the bladder.
Weight management also plays a vital role in alleviating symptoms of overactive bladder. Excess body weight can place additional pressure on the bladder, leading to more frequent urges. Engaging in regular physical activity not only aids in weight loss but also complements bladder exercises by strengthening pelvic floor muscles. This holistic approach toward maintaining a healthy weight can significantly influence bladder control.
Moreover, incorporating stress reduction techniques can profoundly affect one’s ability to manage OAB. Practices such as mindfulness, meditation, and yoga not only help lower stress levels but also promote relaxation of pelvic muscles. This relaxation can help to decrease the frequency or urgency of bladder urges. Establishing a routine that includes these stress-relieving activities may facilitate a supportive environment for exercising the pelvic floor effectively.
Through these combined lifestyle changes, individuals can create a holistic approach that complements their exercises for overactive bladder control, promoting both physical and emotional well-being.
Consulting with Healthcare Professionals
When considering an exercise program for overactive bladder (OAB) control, it is crucial to consult with healthcare professionals. These providers can offer personalized guidance tailored to individual needs and circumstances, which is essential given the complexity of OAB symptoms. Starting an exercise regime without professional advice may lead to ineffective strategies or, in some cases, exacerbate existing symptoms.
During the consultation, patients can openly discuss their symptoms, treatment options, and any concerns they may have regarding physical activities. A thorough assessment by a healthcare provider can identify any underlying health issues that may necessitate a tailored approach to exercise. By sharing specific symptoms, individuals can work collaboratively with their healthcare professionals to develop a comprehensive plan that encompasses both exercise and other therapeutic measures.
In more severe cases of OAB, healthcare professionals might recommend physical therapy or specialized training. These approaches can address the nuances of bladder control and enhance the effectiveness of exercises specifically aimed at managing OAB. Physical therapists, for instance, can provide targeted exercises that strengthen the pelvic floor muscles, contributing substantially to improved bladder control. Additionally, they are equipped to offer guidance on posture and relaxation techniques to further alleviate the symptoms associated with OAB.
Moreover, healthcare professionals are also well-versed in monitoring progress and making necessary adjustments to the exercise program. By collaborating with experienced providers, individuals can optimize their exercise routines, ensuring they are safe and beneficial. It is essential to establish a solid foundation of knowledge and resources to prevent potential setbacks during the journey to managing OAB effectively. Engaging with healthcare professionals not only equips individuals with essential tools but also contributes to fostering a supportive environment that prioritizes health and well-being.
Success Stories and Testimonials
Individuals who have faced the challenges of an overactive bladder (OAB) often draw strength and motivation from the success stories of others who have navigated similar paths. One noteworthy account comes from Sarah, a 45-year-old teacher who struggled with OAB symptoms for years. After discovering a routine that combined pelvic floor exercises with regular walking, she was able to significantly reduce her symptoms. Sarah notes, “At first, I was skeptical about whether exercises could help me regain control, but after a few months, I felt a remarkable improvement in my daily life.” Her story emphasizes the importance of consistency and finding a supportive community to share experiences and tips.
Another inspiring testimonial is from Mark, a 55-year-old retiree who enjoyed an active lifestyle prior to being diagnosed with OAB. He faced the dual challenges of social anxiety and physical limitations. Determined to overcome these obstacles, Mark sought guidance from a physical therapist specializing in bladder health. He incorporated specific exercises targeting the pelvic floor and embraced yoga to promote relaxation. “Exercise not only gave me physical strength but also mental clarity,” Mark shares. “It transformed my outlook and encouraged me to face social situations with confidence.” His journey illustrates how lifestyle changes, paired with targeted exercises, can lead to significant improvements.
Additionally, Emma, a 30-year-old athlete, discovered that modifying her training regimen enabled her to manage her symptoms effectively. “I learned to listen to my body and adapt my workouts when necessary. I found that certain low-impact exercises minimized my urgency,” she recalls. Emma’s proactive approach, alongside her dedication to education about OAB, has empowered her to inspire others facing similar challenges. Through her experience, it becomes evident that sharing strategies can foster a supportive environment that enhances awareness and provides encouragement for those dealing with overactive bladder issues.